The International Association for the Study of Pain defines pain as "an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage". Pain is an important symptom in many medical conditions and can interfere with a horse’s general functioning, performance and quality of life. It is one of the main reasons for horse owners to consult their equine veterinarian but it can be difficult to objectively assess pain, particularly in our non-verbal veterinary patients.

Veterinarians and horse owners are often confronted with painful conditions in horses, varying from lameness to abdominal pain, post-surgical pain or more chronic pain states. Depending on the origin and intensity of pain, effective pain management can be provided either by single medications or with multi-modal analgesia. Dechra offers a comprehensive equine pain management range, helping vets and horse owners to confidently manage each equine patient.
What is essential for effective treatment of pain in horses?
Effective treatment of pain in horses relies upon:
- A good understanding of the underlying mechanisms of pain and the different steps in the pain pathway
- Effective recognition and monitoring of pain in the equine patient
- Availability of effective analgesic drugs, preferentially approved for use in horses
Pain and the pain pathway
What is pain? add
What types of pain are commonly seen in horses? add
There are many different types of pain which can be classified according to origin, location, duration, etc. The types of pain most commonly encountered by equine veterinarians include:
- Lameness (common causes include pain in the foot, limbs and other parts of the musculoskeletal system, eg. the back and neck)
- Abdominal pain (colic)
- Post-surgical pain
- Painful conditions of the eyes or teeth
- Painful skin conditions or wounds
Pain Pathway Processes
Transduction add
Transduction is the process by which noxious stimuli are converted into pain signals which are transmitted via peripheral nerves to the central nervous system (CNS). Initially a noxious stimulus is converted into an electrical signal by activation of nociceptors at peripheral nerve endings. Nociceptors respond to thermal, mechanical or chemical stimulation. Peripheral sensitisation can occur and happens when inflammatory mediators decrease the threshold and sensitivity of nociceptors near the site of injury.
Molecules that target transduction:
Local anaesthetics: mepivacaine (Intra-Epicaine), lidocaine (Lignol)
Opioids: butorphanol (Alvegesic), buprenorphine (Bupredine)
NSAIDs: phenylbutazone (Equipalazone), meloxicam (Meloxidolor or Novaquin)
Transmission add
The pain signal is then transmitted through the sensory nervous system (sensory C and A-delta nerve fibres) to the dorsal horn of the spinal cord via peripheral afferent nerves and dorsal root ganglia.
Molecules that target transmission:
Local anaesthetics : mepivacaine (Intra-Epicaine), lidocaine (Lignol)
Modulation add
Once the signal reaches the dorsal horn of the spinal cord it is modulated. Modulation of noxious information as it enters the dorsal horn of the spinal cord has a significant impact on the degree of pain ultimately perceived by the animal. There are descending adrenergic and serotonergic pathways between the brain and the spinal cord which can be activated and may further modulate the signal in the spinal cord. Spinal cord modulation also affects signal transmission to the brain and how it is ultimately perceived by the brain. When the nervous system becomes regulated in a persistent state of high reactivity this is known as central sensitisation. This can lower the threshold for pain (hyperalgesia) or cause pain to be perceived after a non-painful stimulus (allodynia). The effects of spinal cord modulation may last for hours, days or longer and can be inappropriate for the degree of initial injury. It can also be involved in the development of chronic/neuropathic pain states.
Molecules that target modulation:
Local anaesthetics: mepivacaine (Intra-Epicaine)
Opioids: butorphanol (Alvegesic), buprenorphine (Bupredine)
NSAIDs: phenylbutazone (Equipalazone), meloxicam (Meloxidolor or Novaquin), ketoprofen (Ketodolor)
NMDA receptor antagonists: ketamine (Anesketin)
Alpha-2 agonists: detomidine (Domidine), romifidine, (Rominervin), xylazine (Nerfasin)
Perception add
The signal travels to the brainstem and to the cerebral cortex and higher brain centres where pain is perceived. Until the pain signal reaches the cerebral cortex pain is not perceived. However, even in the anaesthetised animal when pain may not be perceived, the sub-cerebral nociceptive mechanisms continue. This is why reflex responses such as increases in blood pressure may still occur in anaesthetised animals in response to surgical stimulus and why providing effective analgesia (systemically or via regional anaesthesia techniques) is vital even in the anaesthetised patient.
Molecules that target perception:
General anaesthetics: ketamine (Anesketin)
Opioids: butorphanol (Alvegesic) , buprenorphine (Bupredine)
Alpha-2 agonists: detomidine (Domidine), romifidine (Rominervin), xylazine (Nerfasin)
How to recognise pain in the horse?
What are the different types of pain? add
Physiological pain is essential for survival and allows detection and reflex withdrawal from harmful insults. This type of pain is short- lived and the condition quickly returns to normal.
Clinical pain starts with acute trauma or inflammation and can lead to sensitisation of the nociceptive system.
Neuropathic pain may develop from direct trauma to the nervous system itself or may develop from ongoing inflammatory damage due to disproportionate inflammatory response.
Chronic pain may develop from severe inflammatory or neuropathic pain, leading to sometimes irreversible changes to the nervous system and pain that can be very difficult to treat.
These latter forms of pain do not serve any useful purpose and reducing pain to a minimum ensures animal welfare and improves convalescence, resulting in optimisation of treatment success. (Bisgaard et al. 2001, Sellon et al. 2004)
How can Equine Pain Scales help in measuring and monitoring pain? add
As pain is defined as ‘an unpleasant sensory and emotional experience’ it can be difficult to objectively assess pain, particularly in non-verbal veterinary patients.
To date, no universal equine pain scale has been developed. In order to make evaluation of pain as consistent and objective as possible it is important to determine which types of behaviour and physiological parameters are associated with pain, to systematically observe these signs, specify the intensity of pain associated with these signs and combine these findings into a quantitative score. This score can then be used to assess degree of pain over time, determining need for and response to analgesic treatment.
Several different equine pain scoring protocols exist and are generally used for specific types of pain. These vary from simple descriptive scales , to more complex, composite pain scales. Where possible validated pain scales and pain scales appropriate to the type of pain being measured should be used.
Examples of pain scales described for equine patients:
AAEP Lameness Grading Scale: 0-5, used to score lameness (musculoskeletal pain)
Composite Pain Scales:
for orthopaedic pain (Bussières et al. 2008)
for postoperative visceral pain (Graubner et al 2011, van Loon et al.2014)
for post-castration pain (UNESP-Botucatu composite pain scale, Taffarel et al. 2015)
Horse Grimace Scale:
for post-castration pain (Dalla Costa et al. 2014)
for acute laminitis (Dalla Costa et al. 2016)
for experimentally induced pain (The Equine Pain Face ; Gleerup et al. 2015)
EQUUS-FAP (Equine Utrecht University Scale for Facial Assessment of Pain):
for head related pain (van Loon and Van Dierendonck 2017)
for acute visceral pain (Van Dierendonck and van Loon 2016),
for orthopaedic surgery and trauma (van Loon and Van Dierendonck 2019)
Facial expressions of pain have been researched extensively in recent years and form the basis of several pain scales which are validated and easy to use. Horses may display obvious facial expressions associated with pain. These include asymmetrical/low-held ears or ears held stiffly backwards, angled eye/tension above the eye area and orbital tightening, withdrawn appearance, tense stare, nostrils square and ‘strained’, tension of the muzzle and pronounced chin and tension of the chewing muscles. Certain behaviours like moaning, yawning, teeth grinding or flehmen can be expressions of pain as well.
What is important to consider when assessing pain in horses? add
When assessing pain it is important to remember what is normal behaviour for the horse/donkey and to recognise that observing the horse in unfamiliar surroundings (such as the hospital setting) or whilst under the influence of sedative medications can affect pain evaluation. Observing from a distance or via video recording can be helpful in some circumstances. Horses in pain can display certain general pain behaviours and can also display pain-specific behaviours and potentially changes in physiological parameters. Examples of pain-specific behaviours include decreased weight bearing due to orthopaedic pain and pawing, flank-watching and rolling in relation to colic pain. General pain behaviours include; restlessness, depression, decreased activity, decreased appetite and reduced interest in socialisation. Whenever a horse displays a dramatic change in attitude or performance it could be that pain is the underlying cause.
Various physiological parameters have been historically believed to correlate with degree of pain in the horse however studies have shown that this correlation is variable depending on the type of pain in most cases. Non-invasive blood pressure monitoring, serum cortisol and serum endorphins have been shown to correlate with pain but are practically less useful in the clinical setting.

How can EPWA (Equine Pain and Welfare app) help you monitoring pain in your equine patients?
Reliable pain recognition and monitoring are key for optimal pain treatment. EPWA has been developed by researchers from the Faculty of Veterinary Medicine at Utrecht University, in collaboration with De Paardenkamp Foundation and Friends of VetMed. EPWA aims to facilitate the recognition and monitoring of pain with the aim to improve welfare in equids. It provides a simple, accessible tool for clinicians, nurses and horse/donkey owners to be able to objectively measure a horse or donkey’s pain by means of Composite Pain Scale or Facial Expressions.
Dechra proudly supports EPWA.

The Equine Anaesthesia App is back
Clarity not complexity.
It is with great pleasure we inform you that the Dechra Equine Anaesthesia app is available again.
Designed to work hand in hand with Dechra's extensive product range, the app can assist vets to choose optimal anaesthetic protocols, simplify sedation and general anaesthesia procedures and to calculate drug doses and infusion rates quickly and easily.
How to treat pain in the horse
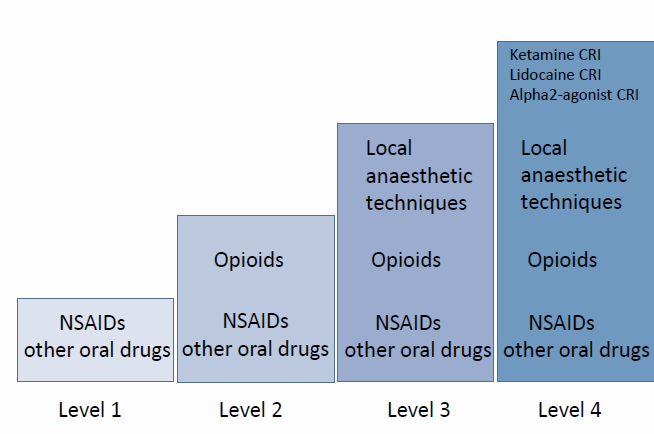
Equine Pain Ladder
NSAIDs add
NSAIDs are the most commonly used analgesic drugs used in horses. They provide predominantly peripheral antinociception by cyclo-oxygenase (COX-1 and COX-2) enzyme inhibition, reducing production of eicosanoids including prostaglandins and thromboxanes which are involved in the inflammatory response. NSAIDs can be administered via injection or orally which makes them useful for treating acute or peri-operative pain as well as for treating more chronic types of pain such as orthopaedic pain. NSAIDs can be associated with renal and gastrointestinal adverse effects due to their effect on prostaglandins involved in homeostatic processes. COX-2 specific or preferential NSAIDs have been developed but a clear clinical benefit of these in the horse has not been shown.
Phenylbutazone (Equipalazone)
Flunixin meglumine
Meloxicam (Novaquin and Meloxidolor)
Ketoprofen (Ketodolor)
Opioids add
Opioids provide the ‘gold-standard’ of analgesia and also can potentiate the effect of sedative drugs. Opioids predominantly provide centrally acting anti-nociception mainly via mu opioid receptors, and their sedative enhancing effects are predominantly mediated by kappa receptors. Opioid receptors are primarily located in the CNS, but can also be found in peripheral tissues, for example in joints. The expression of these peripherally located opioid receptors is upregulated during inflammatory conditions. Opioids affect spinal cord modulation and cerebral control of descending inhibitory pathways and can help to prevent central sensitisation. Opioids can cause side effects such as decreased intestinal motility and increased locomotor activity which has led some people not to use these powerful analgesics in horses. These side effects can usually be effectively managed and are seen less frequently in horses that are in pain (compared to pain-free research horses) or when used in combination with sedatives (such as alpha-2 agonists).
Butorphanol (Alvegesic)
Buprenorphine (Buprenodale/Bupredine)
Methadone (not approved for use in horses)
Morphine (not approved for use in horses)
Alpha-2 agonists add
Alpha-2 agonists are the cornerstone of sedation in horses and also provide analgesia. Adrenoreceptors are found in the dorsal horn of the spinal cord and they affect descending inhibitory medullar pathways. Each alpha-2 agonist has a different duration of action and a different selectivity for stimulation of the alpha2-receptor.
Xylazine (Sedaxylan/Nerfasin)
Detomidine (Domidine)
Romifidine (Rominervin)
Local anaesthetics add
Local anaesthetics block the intracellular sodium channels and thus the development and transmission of an action potential, which leads to anesthesia in sensory fibres. Local anesthetics can be used for local and regional nerve blocks for diagnostic purposes (lameness examinations for instance) or for creating surgical conditions in sedated or anesthetised animals.
Mepivacaine (Intra-Epicaine)
Lidocaine (Lignol)
Courtesy Dr. Thijs van Loon, modification of the WHO Pain Ladder for Humans.
Multimodal Treatment
What is multimodal analgesia? add
Multimodal analgesia is providing a combination of analgesics which act via different mechanisms or on different parts of the pain pathway to provide enhanced analgesia without additional toxicity. The effect is synergistic, or at least additive. For example, combinations of opioids and NSAIDs are commonly used in veterinary species.
Use of several pharmacological classes of analgesic medication at the same time improves overall analgesia whilst allowing lower doses of each medication to reduce side effects.
Selecting appropriate analgesic treatment is assisted by knowledge of the processes involved in the pain pathway. Depending on the origin and intensity of pain, effective pain management can be provided by a single drug or by a combination of different medications and/or administration routes, which target multiple parts of the pain pathway to achieve multimodal analgesia.
How does the anaesthetic protocol chosen affect intra and post- operative pain? add
We know that horses can react to nociceptive stimuli, even when anaesthetised. We also know that inadequate pain relief has been shown to adversely affect outcomes in terms of morbidity, mortality, complication rate, length of hospitalisation and overall cost of treatment in other species and this is likely to be the same for the horse. Not managing pain adequately is likely to adversely affect the nervous system, potentially causing hyperalgesia and allodynia.
Vets should be aware which drugs used in the anaesthetic protocol have analgesic properties eg. alpha-2 agonists, NSAIDs, opioids and ketamine, and which have no analgesic properties eg. acepromazine, midazolam, diazepam, isoflurane. This will allow proper planning of analgesia including preemptive analgesia, administered prior to surgery, and will ensure intra- and post-operative analgesia are provided. Good peri-operative analgesia is likely to smooth maintenance and recovery periods as well as improving overall outcomes.
Regional anaesthetic techniques allow more procedures to be performed during sedated, standing surgery, avoiding the risks associated with general anaesthesia. They also lower the requirement for general anaesthetics when used concurrently during general anaesthesia, improving analgesic efficacy and reducing the incidence of side effects from general anaesthetics.
Summary of key points
- Local anaesthetics: mepivacaine (Intra-Epicaine)
- Opioids: butorphanol (Alvegesic/Morphasol/Torphadine), buprenorphine (Buprenodale or Bupredine)
- NSAIDs: phenylbutazone (Equipalazone), meloxicam (Meloxidolor or Novaquin), ketoprofen (Ketodolor)
- NMDA receptor antagonists: ketamine (Anesketin)
- Alpha-2 agonists: detomidine (Domidine), romifidine, (Rominervin), xylazine (Nerfasin)
References add
-
Bisgaard,T; Kehlet. H. and Rosenberg, J. (2001) ‘Pain and convalescence after laproscopic cholecystectomy’ Eur. J. Surg. 167; pp. 84-96
-
Bussieres, G; Jacques, C; Lainey, O; Beauchamp, G; Leblond, A; Cadore, J.L; Desmaiziéres, L.M; Cuveilliez, S.G. and Troncy, E. (2008) ‘Development of a composite orthopaedic pain scale in horses’ Res. Vet. Sci. 85; pp. 294-306
-
Dalla Costa, E; Minero, M; Lebelt, D; Stucke, D; Canali, E. and Leach, M.C. (2014) ‘Development of the Horse Grimace Scale (HGS) as a pain assessment tool in horses undergoing routine castration’ PLoS One 19:9; pp. 3
-
Dalla Costa, E; Stucke, D; Dai, F; Minero, M; Leach, MC. and Lebelt, D. (2016) ‘Using the Horse Grimace Scale (HGS) to Assess Pain Associated with Acute Laminitis in Horses (Equus caballus)’ Animals 6(8)
-
Gleerup, K,B; Forkman, B; Lindegaard, C. and Andersen, P.H. (2015) ‘An equine pain face’ Vet Anaesth Analg. 42(1); pp. 103-14
-
Graubner, C; Gerber, V; Doherr, M. and Spadavecchia, C. (2011) ‘Clinical application and reliability of a post abdominal surgery pain assessment scale (PASPAS) in horses’ Vet. J. 188(2); pp. 178-183
-
Sellon, D.C; Roberts, M.C; Bilkslager, A.T; Ulibarri, C. and Papich. (2004) ‘Effects of continuous rate infusion of butorphanol on physiologic and outcome variables in horses after celiotomy’ J. Vet. Int. Med. 18; pp. 555-563
-
Taffarel, M.O; Luna, S.P; de Oliveira, F.A; Cardoso, G.S; Alonso, J. M; Pantoja, J.C; Brondani, J.T; Love, E; Taylor, P; White, K and Murrell, J.C. (2015) ‘Refinement and partial validation of the UNESP-Botucatu multidimensional composite pain scale for assessing postoperative pain in horses.’ BMC Vet. Res. 11; pp. 83
-
van Loon, JPAM. and Van Dierendonck, M.C. (2019) ‘Pain assessment in horses after orthopaedic surgery and with orthopaedic trauma’ Vet. J. 246; pp. 85-91
-
van Loon, J,P. and Van Dierendonck, M.C. (2017) ‘Monitoring equine head-related pain with the Equine Utrecht University scale for facial assessment of pain (EQUUS-FAP)’ Vet. J. 220; pp. 88-90
-
van Loon, J.P. and Van Dierendonck, M.C. (2015) ‘Monitoring acute equine visceral pain with the Equine Utrecht University Scale for Composite Pain Assessment (EQUUS-COMPASS) and the Equine Utrecht University Scale for Facial Assessment of Pain (EQUUS-FAP): A scale-construction study’ Vet. J. 206(3); pp. 356-364
-
van Loon, J.P; Jonckheer-Sheehy, V.S; Back, W; van Weeren, P.R. and Hellebrekers L.J. (2014) ‘Monitoring equine visceral pain with a composite pain scale score and correlation with survival after emergency gastrointestinal surgery’ Vet. J. 200(1); pp. 109-115