Treatment of acute cases
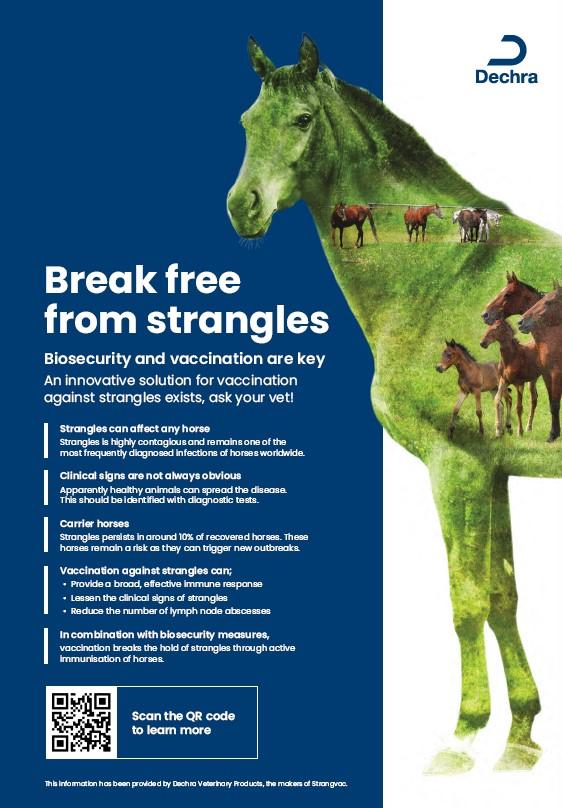
Most infected horses will recover from strangles without treatment, but the recovery period is relatively long and usually takes three to six weeks if no complications occur.
Early treatment of exposed horses revolves around good nursing care to alleviate clinical signs and may include NSAIDs.
Antibiotics (penicillin) may prevent abscess formation but should only be considered very early in the disease process, if at all.
However:
- Lymph node abscesses quickly become so large that antibiotics cannot penetrate to sufficient levels
- Treatment may be required for several weeks and the infection could still flare up again when treatment stops, extending the recovery period
- Antibiotic resistance is emerging (12.5% of UK isolates in one recent study)7
- Antibiotic treatment may interfere with natural immunity8
Severe cases require emergency treatment with antibiotics, corticosteroids and/or surgical intervention (tracheostomy).
Treatment of carriers
- Physical removal of chondroids from the guttural pouches
- Procaine benzylpenicillin administered into guttural pouches
- Systemic antibiotics for two weeks may be warranted
- Repeat endoscopy and lavage to confirm infection-free status