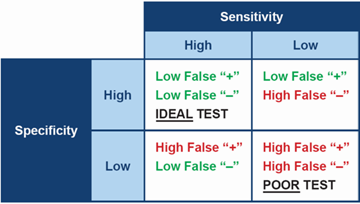
Ideally, when testing for any disease, it is best to choose a test which is both highly specific and highly sensitive. In practical terms, a test with high sensitivity is good at finding animals with the disease and therefore will produce few false negative results. A test with high specificity gives a positive result in animals that really do have the disease, therefore will produce few false positives.
However, no test for Cushing’s has both high sensitivity and high specificity – all are a compromise between the two. This means the diagnostic tests we have for canine hypercortisolism often have to be used in combination, in order to be confident in the diagnosis.
(Please note - the percentage values provided for sensitivity and specificity below should be considered approximate and are representative of multiple investigative studies on this topic. The author refers the reader to the 2019 Bennaim et al review for further information)
ACTH Stimulation Test (ACTHST)
High specificity (90%), moderate sensitivity (85% PDH and 50% ADH)
False positives are less common. False negatives are fairly common.
Low-Dose Dexamethasone Suppression Test (LDDST)
Moderate specificity (70%), high sensitivity (95%).
False positives are fairly common. False negatives are less common.
Urine Cortisol: Creatinine Ratio (UCCR)
Poor specificity (20%), high sensitivity (97%).
False positives are common. False negatives are less common.
When interpreting any of these tests, it is worth considering the positive and negative predictive value. Positive predictive value (PPV) is the fraction of dogs with a positive test that truly have Cushing’s. Negative predictive value (NPV) is the fraction of dogs with a negative test that are truly free of the condition.
The positive and negative predictive values take both the test and the population being tested into account. If you use a test in two populations with different disease prevalence, the predictive values will be different. Therefore the PPV and the NPV vary depend on how frequently you test.
- If we were to test almost every patient we see (a population with a low prevalence - 5%)
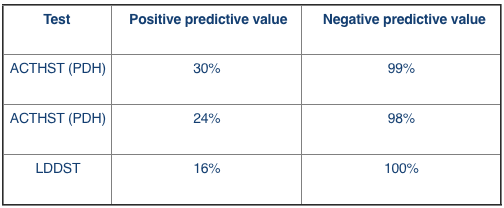
In this scenario, if we use the LDDST we can be 100% sure a negative result is truly negative. However only 16% of positive results will actually have Cushing’s.
- If we were more critical about the patients we test (a population with a high prevelance - 90%)
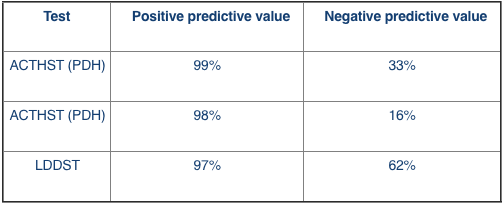
In this scenario, if we use the LDDST, 62% of negative results will truly be negative and 97% of positive results will have Cushing’s.
Conclusion
The 2012 ACVIM Consensus Statement panel (Behrend et al. 2013) considers the low-dose dexamethasone suppression test (LDDST) as the screening test of choice unless iatrogenic Cushing’s is suspected. Because of the ACTH stimulation test’s lower sensitivity its diagnostic usefulness as a screening test for natural occurring Cushing’s syndrome is inferior to the LDDST'.
However, it is also important to take other factors into account when selecting a diagnostic test, including test availability, cost and concurrent disease present in the patient. It is equally important to improve the potential outcome of the test by ensuring there is a high index of suspicion of disease before confirmatory testing is undertaken.